Originally published on 31st May 2017 Last updated on 7th August 2024
As someone who was diagnosed with a ‘borderline underactive thyroid’, I always wince at the phrase.
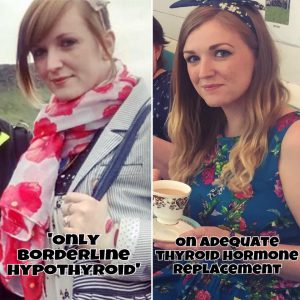
The photo on the left below is from 2015, when I was incredibly ill from ‘only borderline hypothyroidism’, as the doctor kept telling me. You can clearly see that I was not well. I was pale, had huge bags under my eyes and a puffy face.
The photo on the right is two years later, on thyroid hormone replacement.
They refused to treat me for my failing thyroid gland, being destroyed by my own immune system, and dismissed my concerns of feeling overwhelmingly fatigued, weak and unfit. At the end of the day on which this photo was taken, after walking around Edinburgh, I collapsed at the hotel, passing out from pure exhaustion. It took a good hour or so for me to come back around. It was really frightening.
A week later, the doctor eventually agreed to trial me on thyroid hormone replacement and agreed I had autoimmune hypothyroidism now worthy of treatment. Because he let it get that bad. My TSH level still remained ‘borderline’ or ‘subclinical’ yet my symptoms were not ‘borderline’ at all!
‘Borderline’ or ‘Subclinical’ hypothyroidism is a term I am really not keen on, personally. To me, your thyroid hormone levels are either optimal or not.
If they’re not optimal they can cause symptoms and affect your quality of life, so ‘borderline’ levels are no excuse to not treat someone. They are no excuse to withhold crucial medication or imply someone is a hypochondriac. Every person is individual, so we should be treated as such and this includes those with ‘only borderline’ results who have mounting, debilitating symptoms.
Some people will and do feel awful with ‘only borderline’ hypothyroidism.
See Related Posts:
- “Stop Dismissing Thyroid Patients as ‘Only Borderline!”
- Does Borderline Hypothyroidism Need Treatment?
I lost years of my life to thyroid symptoms ruling it, due to doctors dismissing me because they went on inaccurate testing and outdated, wide ranges, above my symptoms (many patients lose many years) until it was so late for me that the medication they did eventually give me made no difference whatsoever. My body was in too poor a state to make use of the T4-only Levothyroxine. I eventually figured out I needed an NDT medication which did help.
As of January 2022, the NICE Guidance states to only consider thyroid hormone replacement medication if TSH is greater than 10 on two separate blood tests, at least 3 months apart. [1]
My TSH was at a 9, with thyroid peroxidase antibodies raging on at >1300 and symptoms debilitating every part of my life. I was barely remaining in work, I was bed bound most days by the fatigue and I had next to no quality of life. I can’t believe we are still going by such a wide range and ignoring the importance of Free T3, Free T4 and thyroid antibodies too.
If your doctor has said you are borderline or subclinically hypothyroid and is withholding treatment, despite your quality of life suffering, I am sorry.
Please consider seeing another doctor who will pay more attention to your symptoms and not just TSH alone.
You should also have a retest of any borderline/subclinical TSH, Free T3 or Free T4 readings to see if they have gotten better or worse. They can occasionally get better, but for many, they get progressively worse. If you wish to order these yourself, please find a link for those in the UK here and a US link here.
Achieving optimal thyroid levels are crucial when recovering your health from poor thyroid function. ‘In range’ is often not enough to remove symptoms. Please see more information on optimal thyroid levels here.
Have you been dismissed with ‘borderline’ hypothyroidism, yet feel very unwell?
You can click on the hyperlinks in the above post to learn more and see references to information given.
The bookBe Your Own Thyroid Advocate: When You’re Sick and Tired of Being Sick and Tired by thyroid patient Rachel, which covers how she got her health back after doctors told her she was ‘only borderline’ hypothyroid.
References:
[1] https://cks.nice.org.uk/topics/hypothyroidism/management/subclinical-hypothyroidism-non-pregnant/